University of Manchester scientists joins three networks to tackle antimicrobial resistance
University of Manchester scientists are part joining three of eight new networks, combining different research specialisms, to tackle one of humanity’s biggest threats, antimicrobial resistance (AMR).
The networks will share £4.8 million from UK Research and Innovation (UKRI), awarded as part of its tackling infections strategic theme. This programme will continue next year with a new opportunity for ambitious new transdisciplinary research programmes, drawing on a dedicated budget of at least £7 million.
The People AMR Network, led by Sarah Tonkin-Crine at The University of Oxford will consider how communities might use antibiotics in the best possible ways to minimise AMR through changing behaviour.
The network will explore ways to help people make decisions about antibiotic use, develop new strategies and tools, and to study these to ensure they target the right people, the right behaviours, and the right settings to have maximum and timely impact at the lowest possible cost. The community will include representatives from the public as well as GPs, dentists, pharmacists, vets and business leaders.
Co-lead Dr Wendy Thompson from The University of Manchester said: “’From antibiotics for a dental abscess through to antifungals for mildew in the bathroom, we just take antimicrobials for granted. Yet the more often we use them for things where they are not strictly necessary, like toothache, the less often they will work when they are vital, like sepsis.
“It’s my pleasure, therefore, to lead the dentistry part of this people-centred approach to helping ensure future generations continue to benefit from antimicrobials that work.”
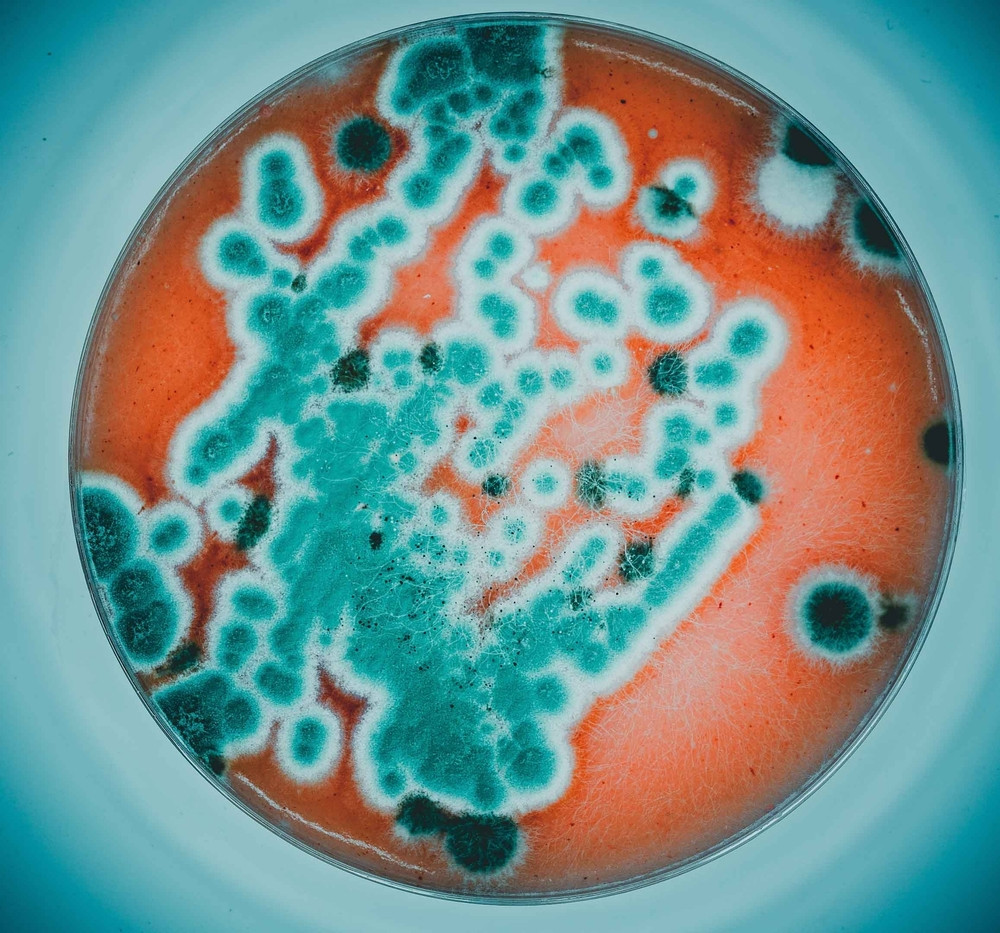
The Fungal One Health and Antimicrobial Resistance Network, led by Darius Armstrong-James at Imperial College London will focus on the emergence of anti-fungal resistance and the development of countermeasures to it, with collaboration from the University of Manchester.
The network will cover healthcare, agricultural and pharmaceutical industries, as well as key government departments and end users in these settings. It will tackle the underlying causes of resistance, surveillance, agricultural waste and water-based hotspots, the development of countermeasures and interventions to mitigate resistance.
Co-lead Dr Michael Bromley from The University of Manchester said: “Fungal pathogens cause devastating losses to all of our staple foods such as wheat, rice, corn, soybean and sugar cane. To combat these losses, which alone are sufficient to feed around half of the world’s population, millions of tonnes of fungicides are sprayed. This widespread and sometimes illegal use has caused drug resistance to emerge in many fungal pathogens of plants, placing pressure on our food security.
“Worse still, these fungicides have caused drug resistance to emerge in human fungal pathogens too. I will be leading a group to understand how we may balance the critical need for fungicide use in crops with the negative impacts they have on driving resistance and how we can work better with Governments to prevent resistance emerging to new the next-generation of antifungals.”
The Accurate, Rapid, Robust and Economical One Health DiagnoSTics for antimicrobial resistance Network will focus on diagnostic tools. It will coordinate and develop practical solutions for diagnostics in both animals and plants, across various settings and is led by Led by Mark Bradley from Queen Mary University of London, with collaborators from the University of Manchester.
This will be addressed by identifying needs across sectors, developing research and innovation, standardising evaluation, supporting implementation, and cross-pollinating findings.
The new networks will support diverse teams of AMR researchers, ranging from specialists in agriculture, food and the environment to human and animal medicine, policy and behavioral studies, engineering and social science. Together they’ll develop new partnerships and approaches to tackling AMR across sectors and disciplines, including culture, economics, behaviour, biomedical and physical sciences, design and engineering, environmental sciences and more.
Dr Colin Miles, Head of Strategy, Advanced Manufacturing and Clean Growth at UKRI, said:
“Tackling the creeping pandemic of anti-microbial resistance – increasing resistance to antibiotics – is a large, complex problem. Ten million people each year are expected to lose their lives to it by 2050.
“Rather than taking single-discipline approaches, we need researchers from across disciplines to come together and look at all aspects of the problem – from human behaviour and how we grow crops and rear animals for consumption to how we manage the environment or use technology, clinical management strategies or challenge established cultural norms.”




