Eleven years ago, myself and my colleagues made an estimation that approximately 2 million individuals across the globe were succumbing to fungal infections on an annual basis. However, my most recent estimation has revealed a staggering increase, with the figure now standing at nearly double that amount: around 3.8 million deaths.
To provide some perspective, this accounts for approximately 6.8% of the total global deaths. The leading cause of death is coronary heart disease, responsible for roughly 16% of the world’s total deaths, followed closely by stroke at 11%. Smoke-related lung disease, also known as COPD, comprises 6% of the total deaths, with fungal infections being accountable for approximately one-third of these 3,228,000 deaths.
When considering other global death statistics, pneumonia claims the lives of 2,600,000 individuals, with some cases being fungal-related, while tuberculosis is responsible for 1,208,000 deaths, of which undiagnosed fungal disease likely contributes to around 340,000 deaths.
These estimates, which have been published in Lancet Infectious Diseases, were reached through careful judgment regarding the proportion of fungal cases that receive proper diagnosis and treatment, as well as those that go unnoticed. Despite significant advancements in fungal disease diagnostics over the past decade or so, both the access to and usage of these tests remain limited, even in countries with higher incomes.
For instance, South Africa is equipped with an excellent diagnostic service for fungal meningitis caused by cryptococcal fungi and bloodstream fungal infections caused by Candida. However, the country lacks diagnostics for infections caused by another prevalent fungus, Aspergillus. These gaps contribute substantially to unnecessary loss of life. Timely diagnosis of severe Aspergillus infections, ideally within 48 hours, could potentially save millions of lives each year.
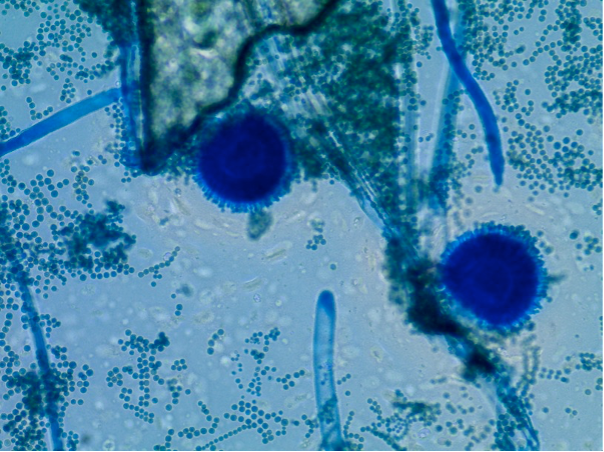
The most critical lethal fungi are Aspergillus fumigatus and Aspergillus flavus, both of which cause lung infections. Those most affected by these infections are individuals with pre-existing lung conditions such as asthma, tuberculosis, and lung cancer. Additionally, individuals who have undergone organ transplants or are in intensive care are also susceptible.
Many of these individuals meet an untimely demise because their doctors fail to recognize the presence of a fungal disease, or they do so too late. However, a significant number of deaths can be attributed to the slow or absent diagnostic testing and the lack of effective antifungal medications. Tests based on fungal cultures only manage to identify approximately one-third of the individuals who are actually suffering from a fungal infection.
Unfortunately, similar to the issue of antibiotic resistance, antifungal resistance is also becoming a growing concern. The use of certain types of fungicides in crop spraying has significantly increased resistance rates to a group of antifungal drugs referred to as azoles.
Infections caused by Candida are a leading cause of sepsis and are found in the bloodstream. These infections are often linked to diabetes or renal failure, or both, and can also occur after major surgeries or traumatic events. Candida is a normal part of the gut microbiome, but when individuals are severely ill, it can cross the gut wall and enter the bloodstream.
With over 1.5 million individuals globally affected by life-threatening Candida infections, resulting in nearly 1 million deaths annually, it is imperative that we develop better diagnostic tests. Current blood culture tests only manage to detect 40% of life-threatening Candida infections.
Approximately 50% of the approximately 600,000 deaths caused by AIDS can be attributed to fungal infections. Significant efforts are being made worldwide to eradicate cryptococcal meningitis as a leading cause of death, with organizations such as the US Centers for Disease Control and Prevention and the World Health Organization taking the lead.
Further work is also required in the field of AIDS, particularly regarding histoplasmosis in Africa and Southeast Asia, where more accurate tests need to be utilized. Many of these patients are misdiagnosed with tuberculosis or have a dual infection with tuberculosis, while the lethal Histoplasma infection remains unrecognized and untreated.
Black fungus
The world witnessed its first large-scale outbreak of mucormycosis, commonly known as black fungus, following the COVID-19 pandemic in India. The fungi causing mucormycosis obstruct the blood supply to tissues, resulting in dead tissue, hence the moniker “black fungus”.
In 2012, my colleagues and I estimated that there were approximately 10,000 cases of mucormycosis worldwide. However, in light of the COVID-19 pandemic in India, the reported cases have skyrocketed to at least 51,000 – a significant increase attributed to factors such as the excessive usage of steroids for COVID-19 treatment and poorly controlled diabetes.
COVID-19 patients in intensive care units around the world have also exhibited a higher incidence of Aspergillus and Candida infections. In fact, the spike in fungal diseases during the COVID-19 pandemic was not taken into account when compiling these newly published incidence and mortality figures, suggesting that the actual numbers could be even higher.
Double whammy
Individuals admitted to intensive care units due to influenza also have a high likelihood of experiencing life-threatening Aspergillus infections, which doubles the risk of death, even if the presence of Aspergillus is diagnosed. Healthcare professionals and scientists are deeply concerned about the possibility of a double whammy epidemic involving fungal infections and influenza or another respiratory virus.
There is also a strong association between fungal allergies and severe, or poorly controlled, asthma.
Asthma is a prevalent condition that becomes increasingly problematic as individuals age. Those with fungal asthma often require multiple medications and experience frequent flare-ups, emergency room visits, and hospitalizations.
Despite the numerous efforts to manage asthma, it is estimated that 461,000 individuals worldwide perish from the condition each year, either directly or as a contributing factor to their final illness.
Fungal diseases are here to stay. They surround us, residing in our guts and on our skin.
There are currently no available vaccines for fungal infections. Severe fungal diseases typically affect individuals who are already ill, with only a few exceptions in healthy individuals or those residing or working in mold-infested homes or environments. This is why accurate and timely diagnosis is of utmost importance, and why we must give fungi the serious attention they deserve.
David W. Denning, Principal Investigator, Manchester Fungal infection Group, University of Manchester
This article has been republished from The Conversation under a Creative Commons license. Read the original article.